🤧 The Allergy Detective: A Guide to IgE, Skin Tests, and the Power of a Trigger Diary
Allergies can feel like a frustrating mystery. The itchy eyes, the random hives, the nagging question of what, exactly, is causing the problem. In the quest for answers, many people turn to broad-panel allergy tests, hoping for a simple solution. But often, the results—a long list of “positive” allergens—only deepen the confusion.
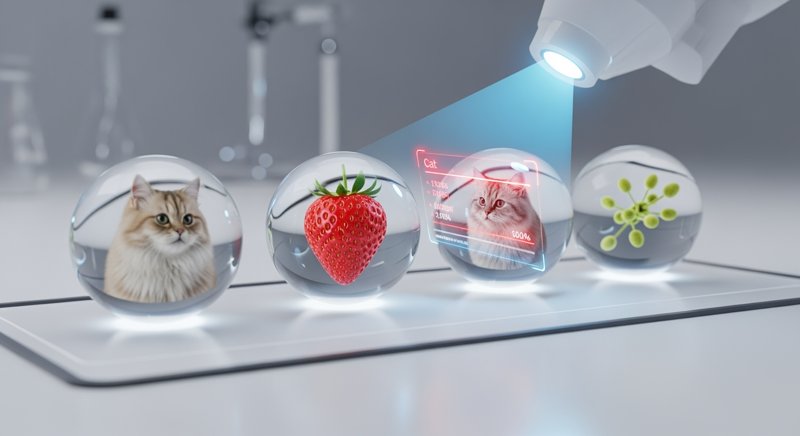
To become a true allergy detective, you need to understand the tools of the trade: what lab tests can and can’t tell you, and why sometimes, the most powerful diagnostic tool is a simple notebook.
The Science of Allergy: Sensitization vs. Clinical Reaction
At its core, an allergy is a case of mistaken identity. Your immune system, in a state of heightened reactivity known as atopy, misidentifies a harmless substance—like pollen, cat dander, or a protein in peanuts—as a dangerous invader.
- The First Encounter (Sensitization): Your immune system produces specific Immunoglobulin E (IgE) antibodies against the allergen. Think of these IgE antibodies as “wanted posters” for that specific substance. They attach themselves to mast cells, a type of immune cell found in your skin, airways, and digestive tract. At this stage, you are sensitized. You have the potential for an allergic reaction, but you won’t experience any symptoms.
- The Second Encounter (Allergic Reaction): When you encounter the allergen again, it binds to the IgE antibodies on your mast cells. This triggers the mast cells to “degranulate”—to release a flood of inflammatory chemicals, most notably histamine. This chemical cascade is what causes the classic symptoms of an allergic reaction: itching, swelling, sneezing, and wheezing.
This two-step process is the key to the entire puzzle: sensitization is not the same as a clinical allergy. You can have IgE antibodies to a substance (a positive test) and yet tolerate it perfectly well in real life. A test result only becomes meaningful when it is correlated with your actual symptoms.
The Diagnostic Toolkit: Unmasking the Suspects
1. Specific IgE Blood Tests
This is a simple blood draw that measures the amount of specific IgE antibodies in your circulation.
- Pros: It’s safe (no direct exposure to the allergen), can be done even if you’re taking antihistamines, and provides a quantitative result that can be tracked over time.
- Cons: It only confirms sensitization. A positive result doesn’t prove that the substance is the cause of your symptoms.
2. Skin Prick Tests (SPT)
A clinician places tiny drops of purified allergen extracts on your skin and makes a small prick. If you are sensitized, a hive-like bump (a wheal and flare) will appear within 15-20 minutes.
- Pros: It’s fast, highly sensitive (especially for environmental allergens), and provides a clear, visual result.
- Cons: You must stop taking antihistamines several days before the test. Like the blood test, it only confirms sensitization.
The Next Frontier: Component-Resolved Diagnostics (CRD)
This advanced form of IgE testing goes a step further. Instead of testing for IgE to “peanut,” it tests for IgE to the specific proteins within the peanut (e.g., Ara h 2, Ara h 8). This is incredibly useful because some proteins are associated with severe, systemic reactions, while others are linked to milder, localized symptoms (like an itchy mouth). CRD helps to distinguish between a true, high-risk allergy and a less dangerous cross-reactivity.
Cross-Reactivity Explained: Sometimes, the proteins in one substance (like birch pollen) are structurally similar to the proteins in another (like an apple). Your IgE antibodies to birch pollen might “mistakenly” react to the apple protein, causing a positive test result and sometimes mild symptoms like an itchy mouth (Oral Allergy Syndrome). CRD can help clarify these complex situations. As of early 2026, molecular allergy diagnostics (including CRD panels) are becoming more widely available through standard allergist referrals, not just specialty research centers.
Beyond IgE: When the Tests Are Negative
What if your IgE and skin tests are negative, but you’re still convinced a certain food is causing problems? You may be dealing with a non-IgE-mediated hypersensitivity. These are true immune reactions, but they involve different parts of the immune system and typically cause delayed, gut-related symptoms (like bloating, pain, or changes in bowel habits). There are no reliable blood tests for these conditions; the diagnosis relies almost entirely on the next tool.
The Ultimate Detective Tool: The Trigger Diary
For many allergic or hypersensitivity conditions, the most powerful diagnostic tool is a well-kept diary.
When the Diary is Your Best Bet:
- Delayed or Vague Symptoms: For issues like eczema, digestive upset, or chronic congestion, a diary can reveal patterns that a one-time lab test will miss.
- Multiple “Positive” Test Results: If your lab report says you’re sensitized to ten different foods, a diary combined with a structured elimination diet is the only way to figure out which, if any, are the true culprits.
- Suspected Non-IgE Reactions: This is the gold standard for diagnosing these conditions.
How to Keep a Diary That Works:
For 2-4 weeks, meticulously log the following:
- Time: When did you eat or get exposed to something?
- Intake/Exposure: What did you eat (list all ingredients), what medications did you take, what was the pollen count?
- Symptoms: What did you feel, how severe was it, and when did it start?
- Context: Note other factors like stress levels, sleep quality, and physical activity.
After a few weeks, you and your doctor can review the diary for correlations. The patterns that emerge are often more revealing than any lab test.
The Strategy: A Detective’s Approach
- Start with the Story: Your clinical history and symptom diary are the foundation.
- Use Tests to Confirm, Not to Fish: Use specific IgE or skin tests to confirm a hypothesis generated by your history (e.g., “I always sneeze around cats, let’s test for cat dander”), not to run a broad, speculative panel.
- Correlate, Correlate, Correlate: A test result is only a clue. It becomes evidence only when it matches your real-world experience.
- Consult the Expert: An allergist is the master detective who can put all these clues together to form a coherent diagnosis and a practical management plan.
Allergy diagnosis is a process of careful investigation. By understanding the tools and playing an active role in the detective work, you can move from a state of confusion to one of clarity and control.




