❤️ Listening to the Heart's Whisper: A Guide to Cardiac Markers in 2025
Medical Disclaimer: This article is for informational purposes only. Cardiac marker tests should only be ordered and interpreted by a qualified healthcare professional in the context of a full clinical evaluation.
The heart, our body’s tireless engine, often works in silence. But when it’s under stress or in trouble, it sends out subtle biochemical signals, whispers that can be detected in a single drop of blood. These signals are cardiac markers, and in 2025, they represent one of the most powerful tools in a cardiologist’s arsenal. They allow us to move beyond the stethoscope and EKG to listen directly to the language of the heart muscle itself.
Understanding these markers is crucial, not just for diagnosing a heart attack in the emergency room, but for predicting risk and managing chronic conditions long before a crisis occurs. Let’s decode the science behind these vital tests.
The Crime Scene Investigators: Markers of Heart Muscle Injury
When heart muscle cells (cardiomyocytes) are deprived of oxygen—the hallmark of a heart attack—they become damaged and release their internal contents into the bloodstream. Cardiac markers are the “biochemical witnesses” to this event.
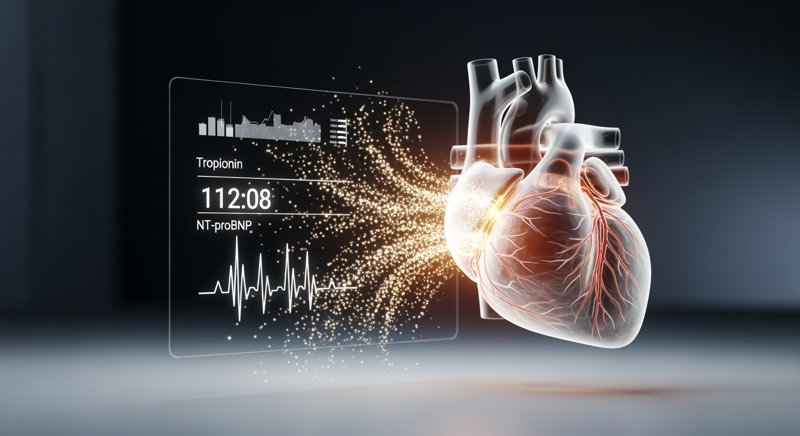
The Gold Standard: High-Sensitivity Troponin
If there is one superstar in the world of cardiac diagnostics, it is troponin. This protein is a fundamental part of the contractile machinery of the heart muscle. Under normal conditions, it stays inside the cells. Its presence in the blood is a direct and highly specific indicator of myocardial injury.
The introduction of high-sensitivity cardiac troponin (hs-cTn) assays has been a game-changer. These tests are so precise they can detect minuscule levels of troponin, allowing for:
- Earlier Diagnosis: A heart attack can be detected within 1-3 hours of symptom onset, a critical time window where rapid treatment saves lives.
- Improved Risk Stratification: Even slight elevations in troponin can predict a higher risk of future cardiac events, helping doctors make crucial decisions about treatment intensity.
According to the latest 2025 guidelines from the American College of Cardiology (ACC) and American Heart Association (AHA), high-sensitivity troponin is the preferred biomarker for the evaluation of acute coronary syndromes.
The Veteran: CK-MB
Before troponin, Creatine Kinase-MB (CK-MB) was the primary marker for diagnosing a heart attack. While it’s less specific than troponin (small amounts can be found in skeletal muscle), it still has a role. CK-MB levels rise and fall more quickly than troponin. This can be useful for detecting a recurrent heart attack that occurs a few days after the first one, a scenario where troponin levels might still be elevated from the initial event.
The Pressure Gauges: Markers of Heart Strain
Not all cardiac markers signal acute damage. Some act as a pressure gauge, revealing when the heart is working too hard.
The Heart’s “Cry for Help”: Natriuretic Peptides (BNP and NT-proBNP)
When the walls of the heart are stretched and strained—a common feature of heart failure—the heart muscle releases hormones called natriuretic peptides (BNP and NT-proBNP). The higher the level of these markers in the blood, the greater the strain on the heart.
These markers are indispensable for:
- Diagnosing Heart Failure: In a patient with shortness of breath, a normal NT-proBNP level can effectively rule out heart failure as the cause.
- Prognosis and Monitoring: In patients with known heart failure, these levels provide a powerful indication of disease severity and the effectiveness of treatment.
The Emerging Biomarker: GDF-15
One of the most exciting new players in 2025 is Growth Differentiation Factor-15 (GDF-15). This protein is released in response to a wide range of cellular stresses, including inflammation and oxidative stress. Elevated levels of GDF-15 are now recognized as a powerful predictor of adverse outcomes across a spectrum of cardiovascular diseases, from heart failure to acute coronary syndromes. As of early 2026, research into GDF-15 has accelerated, with clinical trials exploring its use as a treatment-response marker for emerging heart failure therapies.
The Inflammation Detector: High-Sensitivity C-Reactive Protein (hs-CRP)
We are now beginning to understand that atherosclerosis—the underlying cause of most heart attacks—is not just a plumbing problem of clogged arteries. It’s a chronic inflammatory disease. High-sensitivity C-reactive protein (hs-CRP) is a blood test that measures low-grade inflammation throughout the body.
An elevated hs-CRP level, especially when combined with other risk factors like high cholesterol, signals an increased risk of a future heart attack or stroke. It’s a key part of a comprehensive preventive screening strategy, allowing for more aggressive risk management in seemingly healthy individuals.
A Symphony of Data
The true power of modern cardiac diagnostics lies not in a single test, but in the symphony of information these markers provide. By combining troponin, NT-proBNP, hs-CRP, and a traditional lipid panel, a clinician can build a multi-dimensional picture of your cardiovascular health.
It’s crucial to remember that these tests are powerful tools, but they are not a DIY diagnostic kit. Their interpretation requires a deep understanding of clinical context, and the results must be integrated with your symptoms, physical exam, and other diagnostic tests like an EKG.
The language of the heart is complex, but thanks to the science of cardiac markers, we are learning to listen with ever-increasing clarity. By understanding these whispers, we can intervene earlier, treat more precisely, and empower a future of proactive, personalized cardiovascular care.