⚕️ Decoding Elevated ALT & AST: A Step-by-Step Guide to Your Liver Function Tests
You’ve just received your biochemistry lab report. You scan the results, and suddenly, your eyes lock on two acronyms, ALT and AST, flagged with high values. Your first instinct? A frantic internet search. Fifteen minutes later, you’ve self-diagnosed with cirrhosis, hepatitis, and toxic liver damage.
Let’s take a deep breath. Right now. Slowly. Better? Good.
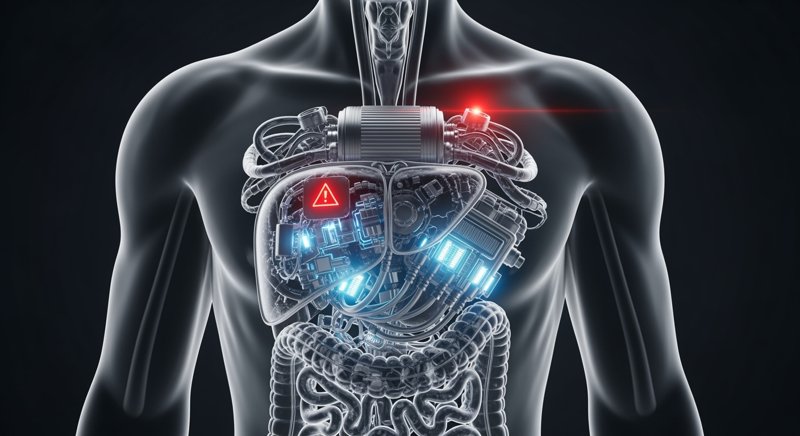
Elevated ALT and AST are not a diagnosis; they are a symptom. Think of them as a warning light on your car’s dashboard. It could signal something as simple as low fuel or as critical as imminent engine failure. To know the difference, you need a mechanic’s perspective. Today, we’ll look under the hood of your body to understand what’s really going on.
What Are ALT and AST, and Where Do They Live?
First, let’s be clear: ALT and AST are not harmful substances. They are enzymes—protein workhorses that live and function inside our cells. Their full names are Alanine Aminotransferase (ALT) and Aspartate Aminotransferase (AST). Their primary job is to facilitate amino acid metabolism, making them vital cogs in our metabolic machinery.
Imagine each cell in your body as a tiny factory, and the enzymes are its workers. As long as the factory walls (the cell membranes) are intact, the workers stay inside, doing their jobs. But if a wall is breached, the workers start spilling out into the street (the bloodstream). The bigger the breach and the more factories are damaged, the larger the crowd of workers on the street.
When your blood is drawn, the lab is essentially counting these “escaped workers.” By their number and specialization, we can deduce which factory has had an accident.
- ALT (Alanine Aminotransferase): This is a specialist, almost exclusively a “liver worker.” The vast majority of ALT is found in liver cells (hepatocytes). Its presence in other organs is minimal. Therefore, high levels of ALT in the blood strongly point to the liver as the source of the problem. It is a highly specific marker for hepatocellular injury.
- AST (Aspartate Aminotransferase): This is a generalist. While also present in the liver, significant amounts of AST reside in the cells of the heart muscle (cardiomyocytes), skeletal muscles, kidneys, and even red blood cells. An increase in AST can signal issues beyond the liver.
Key takeaway: An elevation in ALT/AST almost always signifies that cells are being damaged or destroyed somewhere in the body. Our task is to find out where and why.
Why Are They Elevated? The Main Suspects
The warning light is on. Cells are in distress. Who’s the culprit? The list of suspects is broad, but let’s walk through the most common ones.
1. The Liver: Suspect #1
Since ALT is so liver-specific, it’s the logical place to start.
- Viral Hepatitis (A, B, C, etc.): The classic cause. A virus infiltrates hepatocytes, replicates, and destroys them, leading to a massive “escape” of enzymes. In acute hepatitis, ALT and AST levels can skyrocket to tens or even hundreds of times the upper limit of normal (ULN).
- Non-Alcoholic Fatty Liver Disease (NAFLD): A silent epidemic of the 21st century. Due to metabolic dysfunction—often linked to excess weight, type 2 diabetes, or high cholesterol—fat accumulates in liver cells. A hepatocyte stuffed with fat is like an overpacked suitcase; its membranes stretch and become permeable, allowing ALT and AST to leak out. The elevation is typically mild (2-5x ULN) but persistent.
- Alcoholic Liver Disease: Ethanol and its byproducts are direct toxins to hepatocytes. They cause both fatty changes and direct inflammation (alcoholic hepatitis). Alcoholic liver damage has a characteristic enzymatic signature, which we’ll discuss below.
- Drug-Induced Liver Injury (DILI): The liver is our primary detox organ. It processes everything we ingest, including medications. Some drugs (from high-dose acetaminophen to antibiotics, statins, and antifungals) can be toxic to the liver. Even “harmless” herbal supplements can cause DILI.
- Autoimmune Hepatitis: A rarer condition where the body’s own immune system mistakenly attacks liver cells.
2. Beyond the Liver
If ALT is only slightly elevated but AST is significantly higher, it’s wise to consider other organs.
- The Heart: During a myocardial infarction (heart attack), heart muscle cells die, releasing their large stores of AST into the bloodstream.
- Muscles: Any significant muscle damage—from severe trauma, burns, extreme exercise (CrossFit enthusiasts, take note), or specific muscle diseases (myositis)—will release AST (and another enzyme, CK) into the blood.
Detective Work: Analyzing the Numbers and Ratios
A good clinician acts like a detective when interpreting your ALT/AST levels. They look not just at the absolute values but also at their ratio and other “witnesses” in your lab panel.
The Degree of Elevation
- Mild Elevation (1.5-5x ULN): The most common scenario. It usually points to a chronic, low-grade process like NAFLD, chronic viral hepatitis, or DILI. No need to panic, but investigation is essential.
- Moderate Elevation (5-15x ULN): This suggests a more acute or severe process, such as an exacerbation of chronic hepatitis, more significant DILI, or an autoimmune process.
- Severe Elevation (>15x ULN): This is an SOS signal. It’s most often seen in acute viral hepatitis, severe drug or toxin-induced damage, or ischemic liver injury (a sudden loss of blood flow).
The De Ritis Ratio (AST/ALT)
This is a powerful diagnostic tool. The ratio of these two enzymes can be incredibly revealing.
- AST/ALT < 1: ALT is higher than AST. This is the most common pattern in the majority of liver diseases, including viral hepatitis and NAFLD. Why? ALT is more liver-specific, and it escapes more easily from damaged cell membranes.
- AST/ALT > 2: AST is at least twice as high as ALT. According to the American College of Gastroenterology, this ratio is highly suggestive of alcoholic liver disease. Alcohol damages not just the cell membrane but also the mitochondria—the cell’s powerhouses—where a significant portion of AST resides. This ratio can also indicate the progression to cirrhosis from any cause. And, of course, it points away from the liver and towards the heart or muscles, which contain very little ALT.
Other Clues in Your Bloodwork
ALT and AST are rarely the whole story. To get a complete picture, a physician will look at the entire liver panel:
- GGT and ALP: These are markers of cholestasis, or bile flow obstruction. If they are elevated along with ALT/AST, the problem may involve the bile ducts.
- Bilirubin: This pigment causes jaundice. Its elevation means the liver is struggling to process and excrete it.
- Albumin and PT/INR: These are markers of liver function, not just damage. Albumin is a key protein, and PT/INR measures blood clotting—both are produced by the liver. If these levels are abnormal, it means the factory isn’t just damaged; it’s failing to do its job. This is a very serious sign.
Your Step-by-Step Action Plan
- Step 0: Don’t Panic. A single, mild elevation of transaminases is a reason for investigation, not an immediate cause for alarm. It can even be a lab error.
- Step 1: Be Your Own Sherlock. Before your doctor’s appointment, review the past few weeks.
- Alcohol? Any heavy drinking before the test?
- Medications? Started any new drugs, supplements, or herbal remedies?
- Exercise? Any unusually strenuous workouts?
- Diet? A period of heavy, fatty, or processed food intake?
- Step 2: See a Doctor. Not a forum, not a search engine, but a qualified physician. A primary care provider or a gastroenterologist/hepatologist is your best starting point.
- Step 3: Expect Further Tests. Your doctor will likely order a second round of tests to narrow down the cause:
- Abdominal Ultrasound: To visualize the liver’s structure, check for fat, and rule out obstructions.
- Hepatitis B and C Serology: A standard and essential step.
- A Comprehensive Metabolic Panel: To re-check liver enzymes and assess function markers like bilirubin and albumin.
- FibroScan (Elastography): A non-invasive test to measure liver stiffness, which helps assess for fibrosis or cirrhosis.
In Conclusion
The liver is a remarkably resilient and silent organ. It can endure significant stress without causing any pain (it has no pain receptors). Elevated ALT and AST are often its only way of crying out for help.
Your job is to hear that cry. Not with panic, but with a calm, methodical approach. As of early 2026, updated AASLD guidance continues to emphasize that mild, isolated ALT elevations should prompt repeat testing before invasive workup. Work with your doctor to find the root cause. Remember, most conditions that cause elevated liver enzymes are manageable or reversible with lifestyle changes or treatment.
Understanding your lab results is the first step toward taking control of your health. For a broader perspective on making sense of your reports, see our guide to understanding your medical test results without panic. Since liver health is closely tied to metabolic function, you might also find it useful to learn about understanding your lipid panel.




